
Splitting Ventilators in an Emergency: MADSplit
With COVID19-induced ventilator shortages in Italy and New York, supporting multiple patients on a single ventilator was attempted as an apparently simple solution. The anecdotal use of this approach was also attempted in the 2017 Las Vegas mass shooting event. However, despite these widely publicized attempts, a [joint statement](https://www.apsf.org/wp-content/uploads/news-updates/2020/Multiple-Patients-Single-Vent-Statement.pdf) by the Society of Critical Care Medicine (SCCM), American Association for Respiratory Care (AARC), American Society of Anesthesiologists (ASA), Anesthesia Patient Safety Foundation (APSF), American Association of Critical‐Care Nurses (AACN), and the American College of Chest Physicians (CHEST) all recommended **against** the practice based on safety concerns.
The anecdotal procedure requires "matching" patients, but it remains unclear what this really means. How well do they have to be matched before the benefits to both patients outweigh the risks, especially in rapidly changing pulmonary conditions typical of patients suffering from COVID-19?
***Fundamentally, splitting a ventilator between patients is risky.*** However, should it be absolutely necessary, a potentially reasonable procedure is provided in the following example.
To illustrate the effect of progressive mis-matching, we ventilated two mechanical lungs on a ventilator (840, Puritan Bennett) using pressure control-mode and ARDS-compatible settings (Ppeak=20-30 cmH2O; R =20 bpm; Ftotal=24 L/min; I=1.5 sec; PEEP=8 cmH2O). While keeping patient B at a constant pulmonary compliance (0.03 L/cmH2O), we let patient A progressively deteriorate in compliance from 0.06 to 0.01 L/cmH2O and finally created a maximum mismatch between the patients as shown in the figure.
One-way valves on both inspiratory and expiratory limbs ensured unidirectional flow, which both reduces functional dead-space, risk of cross-contamination between patient A and B and seemingly also facilitated stable ventilation of B as A deteriorated.
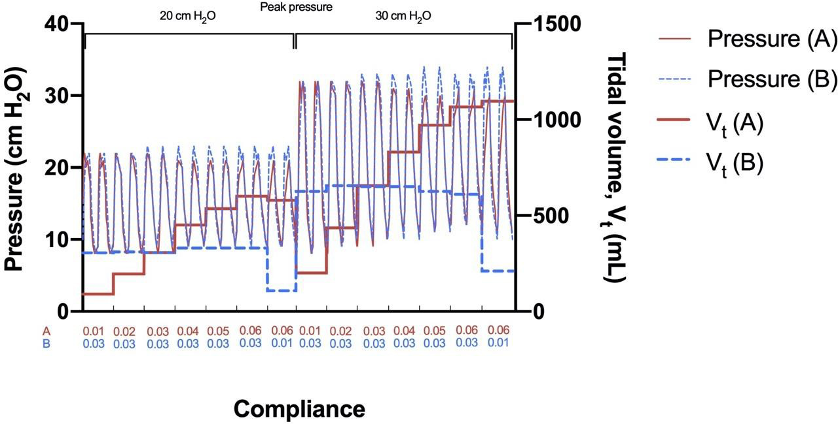
*Figure: Patient A (red line) and B (blue line) pressure curve and average tidal volumes during positive pressure ventilation, pressure control mode mechanical ventilation at 20 and 30 cmH2O and PEEP of 8 cmH2O. One-way valves ensured stable tidal volumes of B while A deteriorated, however, a severe mismatch between the patients could lead to fatal simultaneous hyper- and hypo-ventilation with triggering of alarms.*
Importantly though, **simultaneous and opposite changes in compliance made it possible to fatally hypo-ventilate one patient and hyper-ventilate the other and do so without triggering alarms**, highlighting the danger of splitting a ventilator.
As ventilator alarms are triggered only by changes in the sum of pressure/volume of both patients on the circuit, we instead recommend a narrow alarm range (e.g. Vtidal ±200 mL; Ftotal ±1 L; Ppeak ±5 cmH2O). The one-way valves on each expiratory limb prevented back-flow but introduced a risk of competing exhalation: a slightly earlier or more forceful expiration from A can (partly) impair B and worsen breath-staggering, particularly at higher respiration rates.
Frequent or constant monitoring of patients and shuffling when a mismatch arises is recommended. Asthma or COPD may increase the rate of which fatal mismatch evolves, making the method even more unpredictable. Finally, each class of ventilators requires a specific set up; if the method is considered, use the calm before the patient-surge to familiarize yourself with the ventilators and ameliorate the many risks associated with sharing a ventilator.
This effort was recently accepted for publication in the journal [*Critical Care*](https://ccforum.biomedcentral.com/).
More information is provided via the video below.
Team responsible for this effort

Sidney Merritt
Associate Clinical Professor, Department of Anaesthesiology, UCSD

Aditya Vasan
MADLab PhD student
Mechanical and Aerospace Engineering, UCSD

William Connacher
MADLab PhD student
Mechanical and Aerospace Engineering, UCSD

Lonnie Petersen
MADLab, Center for Medical Devices, Department of Mechanical and Aerospace Engineering, Jacobs School of Engineering, UCSD

Jeremy Sieker
School of Medicine, UCSD
Johan Petersen
Post-doc, Department of Anaesthesiology, UCSD

James Friend
Professor, MADLab, Center for Medical Devices, Department of Mechanical and Aerospace Engineering, Jacobs School of Engineering; Department of Surgery, School of Medicine, UCSD
Gratefully supported by




with funding, facilities, and staff
Our Leadership Team

Lonnie Petersen
Lonnie (MD,PhD) completed her MD from the University of Copenhagen, Denmark in 2007 and has worked in Emergency Medicine and Intensive Care. Dr. Petersen received her PhD in Gravitational Physiology and Space Medicine in 2016. Currently an assistant Professor the University of California, San Diego and supported by NASA, DoD, and the Novo Nordic Foundation as well as being a Sapera Aude Fellow (National Research Council). Her research is rooted in cardiovascular, cerebral and exercise physiology always with an integrative physiology approach.

Casper Petersen
Casper “Johan" (MD) graduated from University of Copenhagen in 2008 and has worked in Cardiology and Emergency Medicine. He has focused on research in renal physiology and sympathetic reflexes as well as physiological fluid shifts in regard to space and aviation medicine and countermeasure development for long term space travel. Dr. Petersen is supported by NASA , Kratos and ONR and currently holds a position as Assistant Project Scientist at University of California, San Diego.

James Friend
James (BSAero, MSME, PhD) leads the Medically Advanced Devices Laboratory in the Center for Medical Devices at the University of California-San Diego. He is a professor in both the Department of Mechanical and Aerospace Engineering, Jacobs School of Engineering, and the Department of Surgery, School of Medicine. He has over 270 peer-reviewed research publications, including 140 journal papers and eight book chapters, and 29 patents in process or granted, completed 34 postgraduate students and supervised 20 postdoctoral staff, and been awarded over $25 million in competitive grant-based research funding over his career. He is a fellow of the IEEE.
Copyright notice
Work(s) (the “Work”) by:
COVID-19 Acute Ventilation Rapid Response Taskforce (AVERT) Medically Advanced Devices Laboratory
Department of Mechanical and Aerospace Engineering
Jacobs School of Engineering and the School of Medicine University of California, San Diego
9500 Gilman Drive MC411
La Jolla, CA 92093-0411
This Work is Copyright © 2020 The Regents of the University of California. All Rights Reserved. Permission to copy, modify, and distribute this Work and its documentation for educational, research and non-profit non-clinical purposes, without fee, and without a written agreement is hereby granted, provided that the above copyright notice, this paragraph and the following three paragraphs appear in all copies. Permission to make commercial and/or clinical use of this Work may be obtained by contacting:
Office of Innovation and Commercialization
9500 Gilman Drive, Mail Code 0910
University of California
La Jolla, CA 92093-0910
(858) 534-5815
innovation@ucsd.edu
This Work and documentation are copyrighted by The Regents of the University of California. The Work and documentation are supplied “as is”, without any accompanying services from The Regents. The Regents does not warrant that the operation of the Work will be uninterrupted or error-free. The end-user understands that the Work was developed for research purposes and is advised not to rely exclusively on the Work for any reason.
IN NO EVENT SHALL THE UNIVERSITY OF CALIFORNIA BE LIABLE TO ANY PARTY FOR DIRECT, INDIRECT, SPECIAL, INCIDENTAL, OR CONSEQUENTIAL DAMAGES, INCLUDING LOST PROFITS, ARISING OUT OF THE USE OF THIS WORK AND ITS DOCUMENTATION, EVEN IF THE UNIVERSITY OF CALIFORNIA HAS BEEN ADVISED OF THE POSSIBILITY OF SUCH DAMAGE. THE UNIVERSITY OF CALIFORNIA SPECIFICALLY DISCLAIMS ANY WARRANTIES, INCLUDING, BUT NOT LIMITED TO, THE IMPLIED WARRANTIES OF MERCHANTABILITY AND FITNESS FOR A PARTICULAR PURPOSE. THE WORK PROVIDED HEREUNDER IS ON AN “AS IS” BASIS, AND THE UNIVERSITY OF CALIFORNIA HAS NO OBLIGATIONS TO PROVIDE MAINTENANCE, SUPPORT, UPDATES, ENHANCEMENTS, OR MODIFICATIONS.
